23 /F female G4P2 L1D1A1 with anaemia and icterus
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.23lcome.
23 yr female with G4P2L1D1A1 was apparently asymptomatic till 4 th month of her 2 nd pregnancy
AOM : 13 yrs Normal regular cycles
Got married to 3 rd degree consanguinity and conceived spontaneous after 6 months of marriage.
Due to absent fetal heart rate induced abortion was done with D and C . All her blood investigations are normal during that period ( records not available)
2 nd pregnancy after 6 months of abortion which is spontaneous and she was normal till 3 rd month of 2 nd pregnancy
During her 4 th month of 2 nd pregnancy she developed yellowish discolouration of eyes , decreased appetite , nausea and vomting - non projectile non bilious not associated with pain abdomen with food as content
She is on regular antenatal checkup in one of the hospitals in miryalaguda where her routine investigations were done then her hb was low 4gm/dl and LFT is dearranged(? indirect hyperbilirubinemia) . 2 blood transfusions were done during her 5 th month cervical cerclage was done. Pt had icterus till the time of delivery. she was referred to higher centre during her 7 th month on 30 th august 2017 i/v/of anaemia- hb 6.8 , TB - 2.4 ,DB -0.8 , sr alb 2.8 , sr lipase 174,PT 17, INR 1.3 . Then she went to Gandhi hospital where 4 blood transfusions done prenatally and she developed sudden onset of labour pains and delivered a male baby pre -term (7 th month) died after 1 month. she received 1 blood transfusion postnatal
she came to our hospital on 3/10/2017 with the complaints of fever, breathlessness, giddiness since 8 days, cough since 3 days.
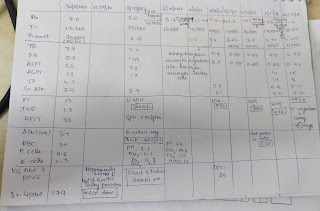
03/10/2017 HB - 3.6 TC-20000
PLATELETS - 2.6
TB - 4.2
DB - 1.49
SGOT - 33
SGPT - 13
Albumin - 3.9
G6PD - 5.8 u/g/hb
RFT - Normal
Serum LDH - 300 IU/L
04/10/2017
PH - 7.1
PCO2 - 11.1
PO2 - 13.7
HCO3 - 3.9
SPO2 - 95.6
05/10/2017
HB - 3.7
TC - 16000
Blood cultures - No growth
06/10/2017
PH -7.4
PCO2 - 19.4
PO2 - 113
HCO3 - 14.2
SPO2 - 98.8
ANA - 48 u/ml
she was diagnosed as autoimmune hemolytic anaemia
? autoimmune pancreatitis ? septic shock with dct and ict positive and started on -inj.monocef 1 gm iv bd -inj.levoflox 500 mg iv od, tab. doxycycline 100 mg bd, -inj. falcigo 500 mg iv bd (28/09/2017 malaria positive) -tab. prednisolone 40 mg od she was admitted her for 3 days and patient was discharged on. -tab. prednisolone 40 mg od,. -tab. orofer xd po od -tab. folvite 5 mg od
she was asked to review after 1 week .
18 October 2017 she visited NIMS in view of yellowish discoloration of eyes since 1 and half month, facial puffiness and pedal oedema since 1 week
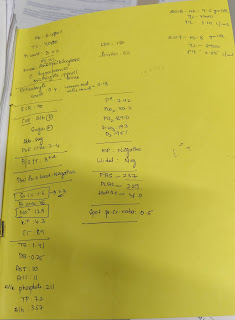
hb - 7.4
tb- 4.0
db- 0.76
tp- 5.0
albumin- 3.1
direct combs test - +2
and kept on. - tab. prediselone 40 mg for 14 days -tab. orofer xd po od -tab. folvite 5 mg od
on 19/ 11/2017 she came to our hospital with swelling over both cheeks since 1 month treatment given. tab. prednisolone 40 mg for 1 month
hb- 11.
19/12/2017 she cane with complaints of facial puffiness, acne, hypertrophy of papillae with ulcer on the tip of tongue tapered the dose of prednisolone from 40 mg to 30 mg she used tab. prednisolone for 3 month
hb- 13.
tb- 3.3
db- 0.5
ldh- 47
she came on 27/2/2018 for reviewOn 27-2-2018
Tab.predinisolone tapered from 20mg for 2 weeks to 15 mg for 2 weeks to 10 mg for 2 weeks to 5 mg for 2 weeks and then to stop it.
On 28-4-2018
she was advised for ANI,lupus anti-coagulant and anti-cardiolipin antibodies testing.
On 12-7-2018
Patient stopped steroids for 2 weeks after developing Cushinoid features for 2 weeks and steroids were started again as 10 mg for 4 weeks
She came in 2019 ,with the C/O 5 months of ameorrhoea and she was Apparently asymptomati
Came for an antenatal checkup with 22 weeks of gestational age.
LMP: 10-7-2019 ,EDD: 17-4-2020
Patient was on Inj prulotin IM weekly once
Tab ecospirin 75 mg OD and Tab susten 200mg B
O/E: Pallor and icterus were present with stable vitals
Referred to GM on 11-12-19 i/v/o hemolytic anaemia and she was advised
tab prednisolone 40 mg OD
Inj vit B12 1000mcg O
On 13-12-19
Thermal amplitude test was positive for cold antibodies
DCT positive,ICT negative
Raised reticulocyte count
Raised bilirubin-> which suggested of cold autoimmune Hemolytic anemia and was advised warm blood transfusion and steroid administration in case of severe hemolysis
28-12-2019
Hb electrophoresis was done which showed Beta-thalassemia
Immunofluorescence showed SPR positive for polymyositis and ANI positive
On 18-1-2020
Cervical encirclage was done i/v/o short cervix with cervical length being 2.5cm, after receiving one PRBC blood transfusion on 4-1-2020
(Hb:8.6gm%
She was diagnosed to have GDM during her 6th month of pregnancy and was kept on MNT for 2 weeks and changed to insulin HAI 6-6-8 UNITS.
24-1-2020
Endocrinologist referreral was taken i/v/o GDM and kept on
Regular: 4-3-3
NPH: 5-x-5
On 26-1-202
Insulin doses were adjusted a
Regular : 6-7-6
NPH:6-x-6
On 21-3-20
Emergency LSCS was done i/v/o oligohydramnios
4 th pregnancy:
6/3/2021
Hb 8.5
TC 7600
plt count 2.7
cue: Alb Nil
pus cells :2-3
LMP lactation ammennorhoea
EDD 1/8/2021 ( 16 wks scan)
POG 33 weeks 1 day
came for cervical cerclage ( short cervix 2.9 cms on TIFFA scan)
No complaints
O/ex pallor ++
iceterus +
no pedal odema ,facial puffiness, generalised lymphadenopathy
HT : 147 cms
wt :37 kgs
BMI 17.1 kg/m2
PR : 100 bpm
BP: 100/70 mm of hg
GRBS :70 gm/dl
spo2 : 98 with RA
CVS : s1,s2
CNS : NAD
R/S : NVBS +
P/A : uterus 22weeks, relaxed
FM +, FP +
FHS + (159 bpm)
suprapubic transverse scar +
6/4/2021
Hb 6.5
TC 8700
plt count 1.5
MCHC
cue: Alb Nil
pus cells :1-2
TB : 3.3
DB :O.77
TP: 5.5
alb: 3.0
Rectic count: 1.8%
sr iron 79 ug/dl
sr ferritin
1 prbc transfusion done on 7/4/2021 hb increased to 8.3 from 6.4
1 prbc transfusion done on 9/4/2021
Diagnosis:
23 F G4P2L1D1A1 with 23 weeks of gestation with AIHA with Beta thalassemia trait



Comments
Post a Comment